Please use this identifier to cite or link to this item:
http://hdl.handle.net/10637/16162Albuminuria-lowering effect of Dapagliflozin, Eplerenone, and their combination in patients with Chronic Kidney Disease: a randomized crossover clinical trial
See/Open:
Albuminuria_Provenzano_JASN_2022.jpg
597 kB
JPEG
See/Open:
Albuminuria_Provenzano_JASN_2022.pdf
Restricted Access
793,85 kB
Adobe PDF
Request a copy
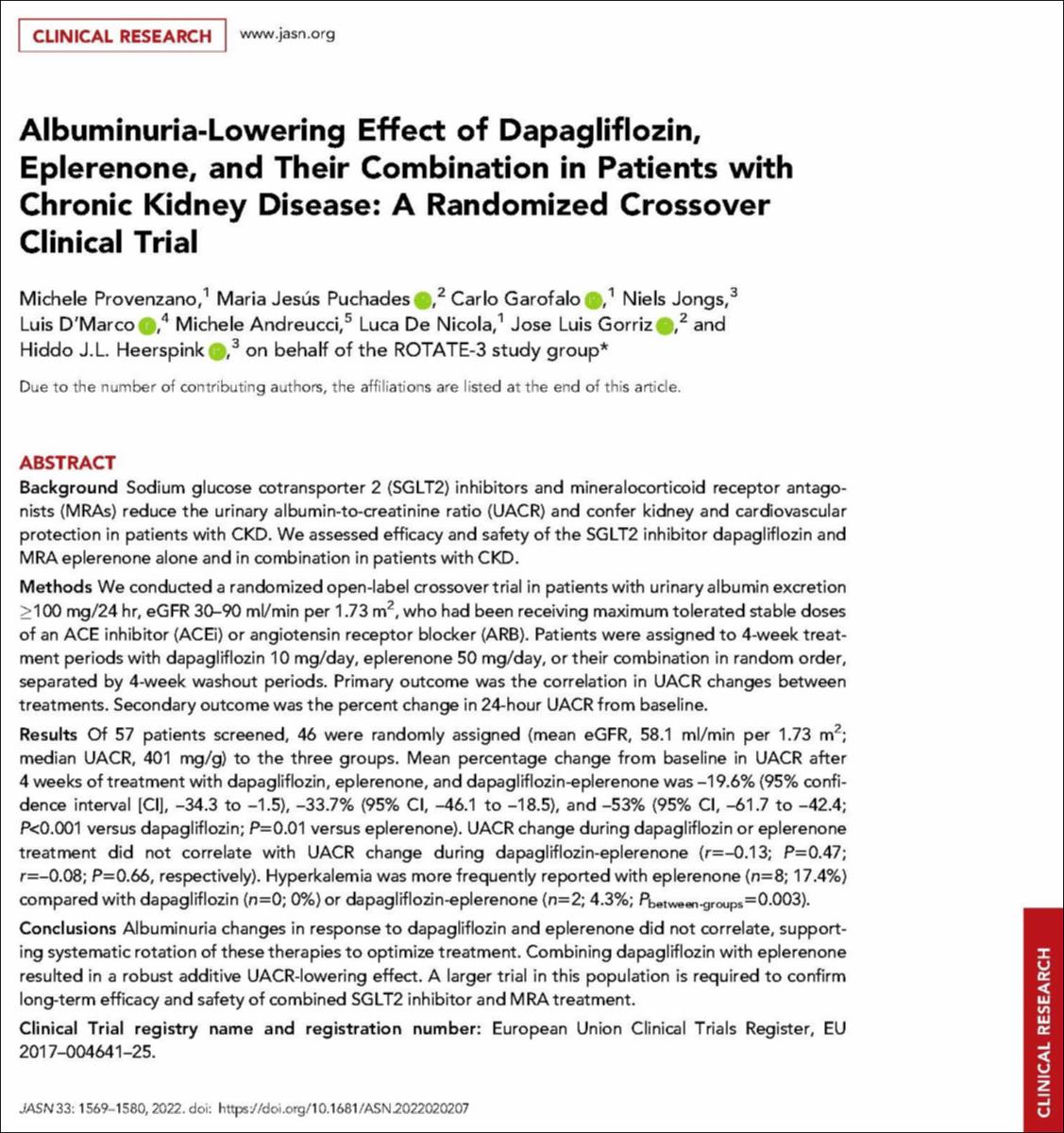
| Title: | Albuminuria-lowering effect of Dapagliflozin, Eplerenone, and their combination in patients with Chronic Kidney Disease: a randomized crossover clinical trial |
| Authors : | Provenzano, Michele Puchades, María Jesús Garofalo, Carlo Jongs, Niels D'Marco Gascón, Luis Gerardo Andreucci, Michele De Nicola, Luca Górriz, José Luis Heerspink, Hiddo J.L. ROTATE-3 study group |
| Keywords: | Albuminuria; Aldosterone; Aldosterona; Urinary system; Aparato urinario; Diseases; Enfermedad; Drugs; Medicamento; Dapagliflozin; Dapagliflozina; Medical treatment; Tratamiento médico; Eplerenone; Eplerenona |
| Publisher: | American Society of Nephrology |
| Citation: | Provenzano, M., Puchades, M.J., Garofalo, C., Jongs, N., D'Marco, L., Andreucci, M., De Nicola, L., Gorriz, J.L., Heerspink, H.J.L. & ROTATE-3 study group members (2022). Albuminuria-lowering effect of Dapagliflozin, Eplerenone, and their combination in patients with Chronic Kidney Disease: a randomized crossover clinical trial. Journal of the American Society of Nephrology, vol. 33, i. 8 (aug.), pp. 1569–1580. DOI: https://doi.org/10.1681/ASN.2022020207 |
| Abstract: | Background: Sodium glucose cotransporter 2 (SGLT2) inhibitors and mineralocorticoid receptor antagonists (MRAs) reduce the urinary albumin-to-creatinine ratio (UACR) and confer kidney and cardiovascular protection in patients with CKD. We assessed efficacy and safety of the SGLT2 inhibitor dapagliflozin and MRA eplerenone alone and in combination in patients with CKD. Methods: We conducted a randomized open-label crossover trial in patients with urinary albumin excretion ≥100 mg/24 hr, eGFR 30-90 ml/min per 1.73 m2, who had been receiving maximum tolerated stable doses of an ACE inhibitor (ACEi) or angiotensin receptor blocker (ARB). Patients were assigned to 4-week treatment periods with dapagliflozin 10 mg/day, eplerenone 50 mg/day, or their combination in random order, separated by 4-week washout periods. Primary outcome was the correlation in UACR changes between treatments. Secondary outcome was the percent change in 24-hour UACR from baseline. Results: Of 57 patients screened, 46 were randomly assigned (mean eGFR, 58.1 ml/min per 1.73 m2; median UACR, 401 mg/g) to the three groups. Mean percentage change from baseline in UACR after 4 weeks of treatment with dapagliflozin, eplerenone, and dapagliflozin-eplerenone was -19.6% (95% confidence interval [CI], -34.3 to -1.5), -33.7% (95% CI, -46.1 to -18.5), and -53% (95% CI, -61.7 to -42.4; P<0.001 versus dapagliflozin; P=0.01 versus eplerenone). UACR change during dapagliflozin or eplerenone treatment did not correlate with UACR change during dapagliflozin-eplerenone (r=-0.13; P=0.47; r=-0.08; P=0.66, respectively). Hyperkalemia was more frequently reported with eplerenone (n=8; 17.4%) compared with dapagliflozin (n=0; 0%) or dapagliflozin-eplerenone (n=2; 4.3%; P between-groups=0.003). Conclusions: Albuminuria changes in response to dapagliflozin and eplerenone did not correlate, supporting systematic rotation of these therapies to optimize treatment. Combining dapagliflozin with eplerenone resulted in a robust additive UACR-lowering effect. A larger trial in this population is required to confirm long-term efficacy and safety of combined SGLT2 inhibitor and MRA treatment. |
| Description: | Este recurso no está disponible en acceso abierto por política de la editorial. |
| URI: | http://hdl.handle.net/10637/16162 |
| Rights : | http://creativecommons.org/licenses/by-nc-nd/4.0/deed.es |
| ISSN: | 1046-6673 1533-3450 (Electrónico) |
| Issue Date: | Aug-2022 |
| Center : | Universidad Cardenal Herrera-CEU |
| Appears in Collections: | Dpto. Medicina y Cirugía |
Items in DSpace are protected by copyright, with all rights reserved, unless otherwise indicated.

